When and how to treat a high baby fever
As a parent, nothing is more precious than your child. If your little one is exhibiting signs and symptoms of a high temperature, your natural reaction might be to panic. It’s normal for your baby’s temperature to fluctuate for various reasons, and it’s not always necessarily bad.
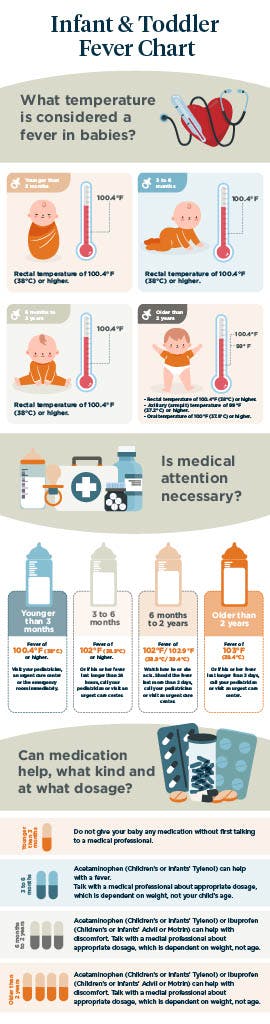
A fever for an infant is defined as a rectal temperature of over 100.4 degrees Fahrenheit or an oral reading above 99 degrees. A fever is typically a symptom of another illness, but knowing exactly what to do can be difficult. Not to worry — you can quickly assess the severity of their fever at home by using a baby fever chart.
Below, we’ll explain the baby fever chart to help you decide whether to treat your little one’s fever at home and when to call the pediatrician or local urgent care center.
What temperature is considered a fever for a baby?
Many people do not know what temperature a fever is for a baby, which is slightly different from what it would be for an adult. This means that parents do not always properly manage the specific situation when a baby has a high temperature.
Your child is considered to have a fever if he or she:
- Has a rectal, ear or temporal artery temperature of 100.4 F (38 C) or higher
- Has an oral temperature of 99 F (37.8 C) or higher
- Has an armpit temperature of 99 F (37.2 C) or higher
If you're unsure about your baby’s temperature reading, use another method to confirm the results.
Infant, toddler and baby fever chart
Measuring your baby’s temperature
You must obtain the right temperature measurement to determine whether your baby has a fever. This starts with having the right instrument. Regardless of your baby’s age, a digital multiuse thermometer is recommended.
Not only is a digital thermometer inexpensive and easy to use, but it’s also the most reliable baby-fever-temperature-taking instrument. There are several ways to take your child’s temperature with a digital thermometer.
- Rectal thermometers: These are recommended whenever possible as they give the most accurate readings, especially for babies and toddlers under 2 years old. However, they typically aren’t fun for you or your baby.
- Armpit thermometers: This method might make obtaining a temperature in your little one easier, but they aren’t as accurate.
- Tympanic (ear) or temporal (forehead) thermometers: These methods aren’t as precise because external temperatures can skew them. Mercury thermometers should be avoided because if they were to break, they would expose your child to their toxic effects.
Since a rectal temperature is considered the most accurate method to assess fever for newborns and babies, this is recommended whenever possible.
How to bring a baby’s fever down
Should your child seem uncomfortable or in pain, there are several options for treating fever in babies at home to help your child feel better.
Fever-reducing medicines such as ibuprofen (for babies over 6 months) and acetaminophen can provide some relief, but other baby fever treatment methods can lower a temperature for babies younger than 6 months old:
- Cold compress: Placing a cool, wet washcloth on your child’s head can draw the fever out and help your baby rest.
- Fluids: To prevent dehydration and aid the body in cooling, give your child plenty of fluids, including water, clear soups, popsicles or yogurt. If your baby is younger than 6 months and you are breastfeeding, breast milk will hydrate and strengthen your little one’s immune system while fighting illness. Formula can also help your baby stay hydrated.
- Keep your baby’s room cool: Use air conditioning or a fan on its low setting to keep your baby’s room at a comfortable temperature (70-74 F). Also, try to avoid taking your child outside in the sun. Should you venture out, remain in the shade.
- Lightweight clothing: Remove extra layers of clothing so your child can lose heat more quickly through the skin. Since infants can’t regulate their temperature well, cooling them down once overheated with multiple layers is harder. Instead, dress your baby in a single layer of light, comfortable clothes and they should sleep with one lightweight blanket.
- Lukewarm sponge bath: Help your child feel more at ease with a relaxing sponge bath using lukewarm water. As water evaporates from your child’s skin, it can bring the fever down temporarily. But avoid using cold water as this can cause your baby to shiver, raising your baby’s temperature.
Whatever you choose to do to alleviate discomfort, do not use aspirin, as this can cause a potentially fatal illness called Reye’s syndrome.
Common causes of fevers in babies and toddlers
It’s important to remember that a fever is not an illness. Instead, it’s a symptom of another underlying issue. In most cases, the issue is probably an infection; however, depending on what type of infection it is or whether it’s another problem will determine the course of treatment.
Some of the most common causes of fever in babies are:
- Viral infection: Viruses like an intestinal infection, the cold, flu, croup or chickenpox can cause your baby to develop a fever as a natural response to fighting off infection. Since viruses are not bacterial in nature, antibiotics will have no effect.
- Bacterial infection: While less typical than viral fevers, bacterial fevers can be more serious. Ear and throat infections, urinary tract infections, bacterial pneumonia or bacterial meningitis require antibiotics to prevent additional health complications.
- Over-bundling: Because they can’t regulate their bodies as well as older kids, infants — particularly newborns — can get fevers if they’re overdressed or in a warm environment. Make sure your baby is not over-bundled with extra blankets or clothes, causing a rise in body temperature. Also, check to see that your baby’s room is comfortable.
- Immunization: If your child received a vaccination in the past 24 hours, they might experience a low-grade fever. This should be nothing to worry about, and appropriate dosages of infants’ or children’s acetaminophen or ibuprofen can be used to alleviate pain. But, if the fever persists past 48 hours, you should call your doctor or visit an urgent care center.
- Teething: It’s possible for your infant to develop a slight rise in temperature because of new teeth. Rubbing your child’s teeth or using a teething ring can help. Seek medical advice if your baby’s teething fever lasts longer than two days.
It can be difficult to determine what is causing the fever, which is why if a fever persists, your healthcare provider may order a blood, urine test or X-ray to pinpoint the root cause.
Seeking medical treatment for your baby’s fever
Let’s say your little one is showing signs of a fever, and you take your child’s temperature. Just because your thermometer reads 102 F, it shouldn’t be cause for alarm. Some parents don’t know that a higher temperature reading doesn’t necessarily correlate to a sicker child.
How do you know if you should call your pediatrician, visit an urgent care center or take your baby to the emergency room?
When to go to the emergency room
Take your child to the emergency room right away or call 911 if they have any of the following symptoms:
- Has a seizure
- Has purple or blood-colored spots on their skin
- Is having trouble breathing
- Is lethargic or not responsive
- Shows signs of dehydration, such as fewer wet diapers, crying without tears or having a sunken soft spot on their head
These symptoms indicate that your baby’s fever is serious and should be treated urgently.
FAQs about fevers in babies
Here are some frequently asked questions about fevers in babies.
How should I dress a baby with a fever at night?
If your baby has a fever or chills, it might be tempting to dress them in extra clothes and blankets. However, doing this may prevent the fever from coming down or increase it, adding to your child’s discomfort.
Instead, dress your baby in a single layer of light, comfortable clothes and your baby should sleep with one lightweight blanket. Keep their room temperature comfortable.
What foods or drinks should I not give my baby while they have a fever?
A baby with a fever may not have much of an appetite, but staying hydrated is essential. Breast milk or formula is ideal for a baby with a fever. If they are vomiting, check with your healthcare provider if they recommend an electrolyte drink like Pedialyte. Do not give a baby fruit juice or other sugar-sweetened beverages.
If your baby is eating solids, it is best to let them eat what they want when they have a fever. Children typically like bland foods such as bread, pasta and crackers. Do not force them to eat.
Can babies get a fever from teething?
Teething does not cause a fever, but can sometimes cause a low-grade elevated temperature. The temperature of a teething infant typically does not go high enough to be defined as a fever.
When to go to urgent care
If a child is not having emergency symptoms related to their fever, they might be able to get treatment at an urgent care, which can save you time and money. Rather than basing the severity of your child’s fever on just a thermometer reading, be aware of your little one’s actions, as this can be a more telling sign of what is happening.
However, you should call your doctor or urgent care center if your baby:
- Has a rash
- Is not eating
- Is not sleeping well
- Is very cranky, irritable or difficult to calm down
You know your baby better than anyone. If you’re ever in doubt, it’s always best to play it safe and call your pediatrician or local urgent care for advice.
Our urgent care partners have visit times available when you can’t wait for your primary care provider. Just walk in or save your spot online at our conveniently located centers. See our prices on co-pays and same-day visits, with and without insurance.
References
- https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/thermometer/art-20047410
- https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Fever-and-Your-Baby.aspx
- https://www.parents.com/health/fever/the-best-way-to-take-a-temperature/
- https://www.ninds.nih.gov/health-information/disorders/reyes-syndrome
- https://medlineplus.gov/ency/patientinstructions/000319.htm
- https://pubmed.ncbi.nlm.nih.gov/10742315/
Written by Sarah Thebarge, Physician Assistant